Connect With Us

Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Foot Strengthening Exercises for Runners

In the world of running, the strength and flexibility of the feet often go unnoticed. From simple toe squish and toe splay exercises to deep squats and hip mobilization techniques, maintaining optimal foot function is essential for improving performance and avoiding injuries. These foot exercises not only strengthen the muscles and ligaments that support the arches, they also encourage proper alignment and biomechanics. Additionally, incorporating jumping exercises can enhance foot elasticity and running efficiency. Whether it's fine-tuning foot mechanics or overcoming injuries, a podiatrist's expertise can be indispensable for runners striving for peak performance and long-term foot health. It is suggested that you make an appointment with a podiatrist who can accurately diagnose any foot problems and offer treatment options to keep you running on the right path.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact one of our podiatrists from David A. Scalzo, DPM, PC and Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctors to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our offices located in Duryea and Bangor, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Exercise for Your Feet
Whether your feet are over-worked or under-worked, chances are they could benefit from some special attention. Even those who exercise regularly probably do not spend any time strengthening their feet. This can be just as rewarding as strengthening the rest of the body, since the health of your feet affects the health of the rest of the body as well, especially the ankles, legs, and spine.
For those who might not have any idea on how a foot-specific exercise might be conducted, there are several workouts that are fairly easy to perform in the comfort of ones’ home. One of the easiest is the toe rise, also known as the tip-toe. This exercise involves standing on the tip-toes for a count of 15 then resting the feet on the ground. This process should be repeated a minimum of three times a day in order to strengthen the feet.
Toe pick-ups strengthen the feet by working them in a very different way. In this exercise, small items are picked up using the toes in order to strengthen the muscles on the upper part of the feet. Once again three sets should be performed, with the item in question being held for 15 seconds then dropped. Items that may be picked up using the feet include marbles and even stationery, which works wonders for the toes and the surrounding muscles.
Yet another simple workout is the ankle pump. This can be done either upwards or downwards, but for the workout to be most effective both can be incorporated into the routine. As the term suggests, this involves lifting the foot off the floor and flexing the toes either towards the shin or towards the ground. This movement puts the feet and ankles through a large range of motion which works the muscles.
Last but not least, feet should be stretched so that the muscles can relax and recuperate. This can be done by placing both feet off of the floor and bracing oneself against the wall at a 45 degree angle. This ensures that the feet and ankles are adequately stretched once the workout is complete.
In short, giving the feet a good workout every now and then is important in order to avoid problems such as plantar fasciitis. It’s also important to warm-up or cool-down after running or vigorous walking. Foot exercises may be followed by a good foot massage. This encourages circulation in the feet as well as muscle relaxation.
Injury Prevention for Runners

All runners are susceptible to a range of foot injuries stemming from the repetitive nature of running and other factors. Neglecting flexibility training can lead to decreased range of motion and increased risk of injuries such as strains and tears. Cross-training, incorporating activities like swimming or cycling, can mitigate these risks by engaging different muscle groups and reducing overuse injuries. Additionally, a balanced approach to fitness will help prevent foot injuries. Podiatrists play a significant role in this respect, offering expertise in foot and lower limb biomechanics, gait analysis, and injury prevention. They can guide proper footwear selection, orthotic devices, and personalized exercise regimens to address individual needs and reduce injury risk. If you are a runner, it is suggested that you make an appointment with a podiatrist to learn more about injury prevention in running so you can enjoy this port for the long term.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact one of our podiatrists of David A. Scalzo, DPM, PC and Associates. Our doctors will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our offices located in Duryea and Bangor, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Prevent Running Injuries
Overtraining and overusing the feet are the main causes of common running injuries. A number of these common injuries are caused by overrunning. Runner’s knee is a condition that is characterized by the back of the kneecap beginning to wear away and cause pain in the knee. This frequently occurs due to either a decrease in strength in the quadriceps muscles or ill-fitting shoes that are lacking in proper support for the inside of the forefoot. Strengthening exercises focusing on the quad muscle and sports orthotics are the usual treatments for those suffering from runner’s knee. Prevention of the condition lies in a focus on hip strengthening and quad-strengthening to keep the kneecap aligned. To help learn the best exercise to heal runner’s knee, one can also undergo physical therapy.
One common injury, called iliotibial band syndrome, is often caused by overtraining. This condition occurs when the iliotibial band gets irritated, creating pain and discomfort in the outside knee area. Plantar fasciitis, another common running injury, also occurs as a result of inflammation and irritation. Plantar fasciitis is an inflammation and irritation of the bone in the foot. A large amount of pain is often experienced due to plantar fasciitis. The condition can be caused by a high arch, improper footwear, tight muscles, or flat feet. It can best be avoided by stretching and wearing appropriate footwear that supports the foot.
Another common injury for runners is stress fractures. These injuries occur due to running style, overtraining, or a lack of calcium. Stress fractures most often occur in several locations in runners, including the inner bone of the leg, the thighbone, the bone at the base of the spine and the bones of the toes. Stress fractures are best prevented by wearing proper footwear and by running on flat and hard surfaces; this will absorb some of the shock created during running.
Aside from overtraining, other causes of common running injuries include ill-fitting footwear, a lack of flexibility and strength, and irregular biomechanics. The best way to avoid running injuries is to prevent them from even occurring. Both iliotibial band syndrome and stress fractures are preventable. The first step that should be taken to prevent running injuries is to only wear footwear that fits properly and that is appropriate for whatever activity you are doing. Running shoes are the only protective gear available to runners that can safeguard them from sustaining injuries. Choosing the right pair of shoes is therefore extremely important. While running shoes are an important factor, it is also important to consider other facets of your running routine such as training schedules, flexibility, and strengthening. These elements should be considered and altered according to your running needs to best maximize your run and minimize the possibility of injury. Careful stretching before and after a run should also be considered to help prevent running injuries. Stretching muscles enables greater flexibility and a lesser chance of sustaining injury.
Common Causes of Plantar Fasciitis
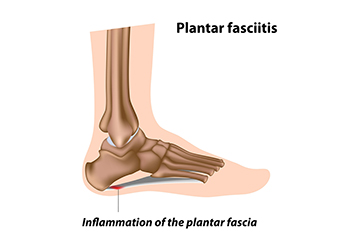
Plantar fasciitis, a common cause of heel pain, can arise from various factors related to foot mechanics, lifestyle, and health conditions. One primary cause is repetitive strain on the plantar fascia, the thick band of tissue that supports the arch of the foot. Activities such as running, walking, or standing for prolonged periods can put stress on the plantar fascia, leading to microtears and inflammation. Poor foot mechanics, including high arches, flat feet, or abnormal walking patterns, can also contribute to the development of plantar fasciitis by placing excess strain on the plantar fascia. Additionally, wearing unsupportive footwear or suddenly increasing activity levels can exacerbate the condition. Certain risk factors such as obesity, age, and occupations that require standing or walking for extended periods of time can increase susceptibility to plantar fasciitis. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can effectively treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from David A. Scalzo, DPM, PC and Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Duryea and Bangor, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Foot Pain as an Early Sign of Rheumatoid Arthritis
 Foot pain can serve as an early warning sign of rheumatoid arthritis, or RA, a chronic autoimmune condition that affects joints. RA can affect the small joints in the feet, leading to swelling, tenderness, and stiffness. For many patients, the feet are the first site of RA-associated joint pain. People may experience pain in the joints of the toes or the middle of the foot, which is often worse in the morning. Typically, both feet are affected. Early intervention is important, as RA can progress to affect multiple joints, which leads to deformities and functional limitations. If you have foot pain or diagnosed rheumatoid arthritis, it is suggested you are under the care of a podiatrist who can offer tailored treatment for the feet.
Foot pain can serve as an early warning sign of rheumatoid arthritis, or RA, a chronic autoimmune condition that affects joints. RA can affect the small joints in the feet, leading to swelling, tenderness, and stiffness. For many patients, the feet are the first site of RA-associated joint pain. People may experience pain in the joints of the toes or the middle of the foot, which is often worse in the morning. Typically, both feet are affected. Early intervention is important, as RA can progress to affect multiple joints, which leads to deformities and functional limitations. If you have foot pain or diagnosed rheumatoid arthritis, it is suggested you are under the care of a podiatrist who can offer tailored treatment for the feet.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact one of our podiatrists of David A. Scalzo, DPM, PC and Associates. Our doctors will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our offices located in Duryea and Bangor, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.