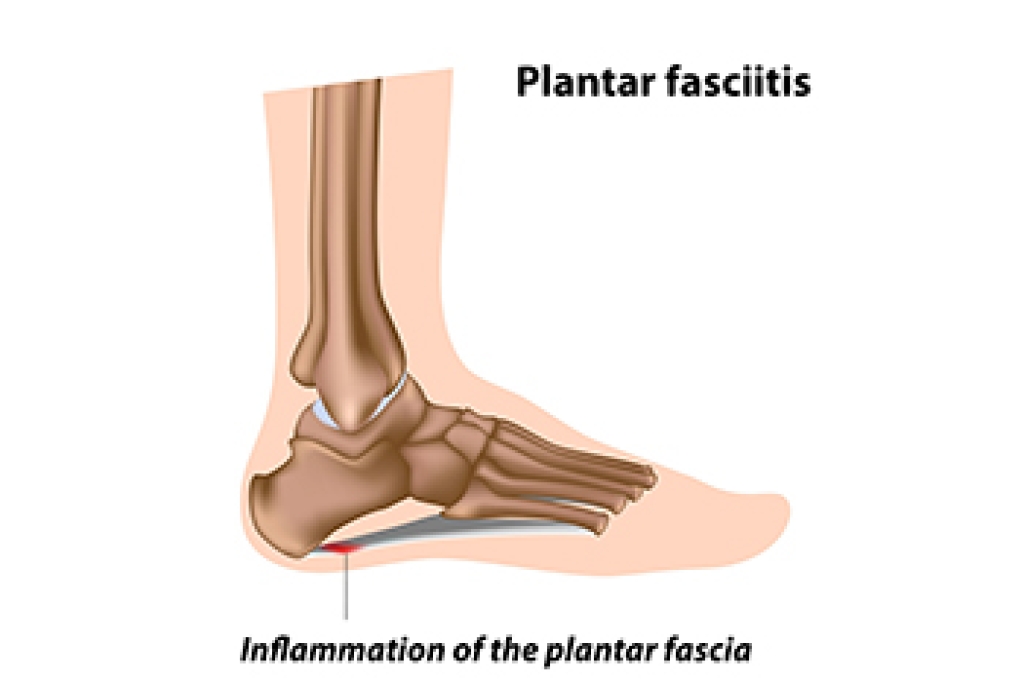
Plantar fasciitis, a common cause of heel pain, can arise from various factors related to foot mechanics, lifestyle, and health conditions. One primary cause is repetitive strain on the plantar fascia, the thick band of tissue that supports the arch of the foot. Activities such as running, walking, or standing for prolonged periods can put stress on the plantar fascia, leading to microtears and inflammation. Poor foot mechanics, including high arches, flat feet, or abnormal walking patterns, can also contribute to the development of plantar fasciitis by placing excess strain on the plantar fascia. Additionally, wearing unsupportive footwear or suddenly increasing activity levels can exacerbate the condition. Certain risk factors such as obesity, age, and occupations that require standing or walking for extended periods of time can increase susceptibility to plantar fasciitis. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can effectively treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from David A. Scalzo, DPM, PC and Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Duryea and Bangor, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.